According to a study by the American Heart Association, nearly 23% of adults experience varicose veins. This vascular condition can affect self-esteem and emotional and physical well-being, especially if you experience unrelenting symptoms such as heavy legs, itching, or pain. At Tennessee Vein Center, our expert team offers advanced, minimally invasive options to restore comfort and confidence. If you or a loved one is seeking the best varicose vein treatment near Knoxville, schedule a consultation today.
What are Varicose Veins?
Varicose veins are enlarged, twisted veins that appear in the calves and thighs.
They often have a blueish-purple hue resembling a knot or piece of rope. It’s important to know that any vein near the skin’s surface can become varicose, not just those in the legs.

Causes of Varicose Veins
Varicose veins are abnormal veins of the superficial venous system that are not functioning correctly and do not return blood to the heart. This failure often results from broken one-way valves, weakened vein walls, or both.
When functioning poorly, these veins allow blood to flow backward, leading to pooling and pressure. Over time, this causes vein walls to stretch and bulge, creating the visible signs of varicose veins.
Risk Factors
Anyone can develop varicose veins, but certain factors increase your risk, including:
- Women, especially those who are pregnant or in menopause
- Individuals who are overweight or obese.
- People who sit or stand for long periods.
- Adults over age 50.
- Those with a family history of vein disorders.
Understanding your risk of developing a vein condition is the first step to optimal vascular health. Book a vein evaluation to learn more about your risks and how to get rid of varicose veins safely and effectively.
Varicose Vein Symptoms
Varicose veins often appear enlarged, twisted, and bulging on the calves and thighs.
Many become more prominent with prolonged sitting or standing.
Problem varicose veins may not be visible on the skin surface. However, they may still cause bursts of abnormal red, purple, or blue smaller veins, leg symptoms, and skin changes associated with venous insufficiency.
In addition to being unsightly, varicose veins are commonly associated with the following symptoms:
- Pain, throbbing, or cramping
- Tiredness and fatigue
- Itching and burning
- Swelling of the ankles and legs
- Heaviness
- Restlessness (Restless Legs Syndrome)
- Swelling or edema of the ankles and legs
In rare instances, people do not experience any symptoms at all.
Varicose Vein Treatment
Our experienced providers offer a wide range of varicose vein treatment solutions to improve circulation and reduce symptoms.
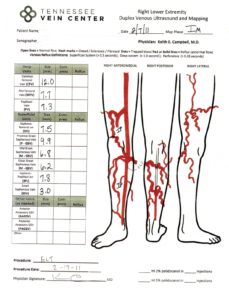
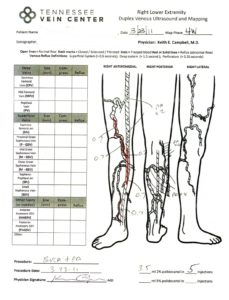
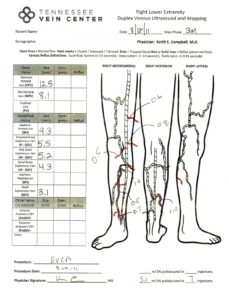
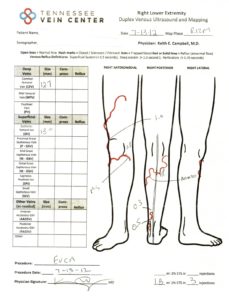
Before initiating any vein treatment of the legs, we perform a screening duplex venous ultrasound, as indicated by your history and exam.
Vein mapping can identify whether underlying veins are not functioning properly and determine the overall severity of the problem. After the mapping, each patient receives a comprehensive treatment plan.
Treatment may include:
- Endovenous Thermal Ablation: A minimally invasive procedure that seals off faulty veins using heat.
- Ultrasound-Guided and Visual Sclerotherapy: Injection treatments to collapse and eliminate diseased veins.
- Veinwave: Ideal for smaller or delicate veins.
- Varithena: A non-thermal injectable foam for hard-to-reach or recurring varicose veins.
- Cutera® Excel V™: A laser-based treatment option for vascular lesions and veins close to the skin surface.
Want to know which option is right for you? Call our office at (865) 233-5858 to speak with a specialist about varicose vein removal options.
The outside of the leg does not have to look terrible for the veins below the surface to be considered insufficient. The maps below show treatment progression and a before-treatment and after-treatment picture of the leg with venous disease.

What Happens if Varicose Veins Aren’t Treated?
Left untreated, varicose veins may lead to more serious complications, including:
- Venous ulcers
- Bleeding
- Skin discoloration
- Deep vein thrombosis (DVT)
- Pulmonary embolism
Early intervention makes a difference. Protect your health and explore minimally invasive varicose vein treatment today.
Effective and Minimally Invasive Varicose Vein Treatment in the Volunteer State
Whether managing early-stage symptoms or dealing with severe varicose veins, Tennessee Vein Center provides leading-edge treatment in a comfortable, patient-first setting.
We combine diagnostic precision with aesthetic expertise to help you feel better, look better, and reduce your risk of long-term complications.
Schedule your consultation today and take the first step toward healthier circulation and a more confident you.
Real Patient Stories
Muffin’s Journey Through Varicose Veins
Muffin is a breast cancer survivor. As such, she carries a lot of traumatic memories from her fight against the disease. To be specific, that fight included a partial mastectomy, a total of 46 radiation treatments, 12 rounds of chemo and 400 chemo pills. There was plenty to be nervous about when Muffin considered stepping back into a medical office for vein treatment.
But much to her surprise, she found great comfort in Tennessee Vein Center and Dr. Campbell, who makes it a priority to make his patients feel comfortable and at ease. Don’t take our word for it, though, you can listen to Muffin’s own words:
You can experience Muffin’s full story by clicking here.
Beverly’s Struggle With Ulcers
Beverly is a big fan of her life in the Great Smoky Mountains. She looks through her kitchen window almost every day to see miles of uninterrupted forest lines — a welcome change from her life in the city. But as she grew older, Beverly developed an ulcer on her leg that would quickly grow from the size of a quarter to the size of a fist.
She tried some vein surgeries, but like many patients, the ulcer eventually returned. This is when she came to see Dr. Campbell at Tennessee Vein Center. As she says herself, she couldn’t have been happier with the treatment she received.
You can experience Beverly’s full story by clicking here.